Jumat, 02 Juli 2010
BID'AH
Al Allamah Asy Syaikh Abdurrahman bin Nashir As Sa`di rahimahullah memaparkan tentang bid`ah : "Bid`ah adalah perkara yang diada-adakan dalam agama. Sesungguhnya agama itu adalah apa yang datangnya dari Nabi shallallahu 'alaihi wasallam sebagaimana termaktub dalam Al Qur'an dan As Sunnah. Dengan demikian apa yang ditunjukkan oleh Al Qur'an dan As Sunnah itulah agama dan apa yang menyelisihi Al Qur'an dan As Sunnah berarti perkara itu adalah bid`ah. Ini merupakan defenisi yang mencakup dalam penjabaran arti bid`ah. Sementara bid`ah itu dari sisi keadaannya terbagi dua :
Pertama : Bid`ah I'tiqad (bid`ah yang bersangkutan dengan keyakinan)
Bid`ah ini juga diistilahkan bid`ah qauliyah (bid`ah dalam hal pendapat) dan yang menjadi patokannya adalah sabda Rasulullah shallallahu alaihi wasallam yang diriwayatkan dalam kitab sunan :
"Umat ini akan terpecah menjadi 73 golongan, semuanya berada dalam neraka kecuali satu golongan".
Para shahabat bertanya : "Siapa golongan yang satu itu wahai Rasulullah ?.
Beliau menjawab : "Mereka yang berpegang dengan apa yang aku berada di atasnya pada hari ini dan juga para shahabatku".
Yang selamat dari perbuatan bid`ah ini hanyalah ahlus sunnah wal jama`ah yang mereka itu berpegang dengan ajaran Nabi shallallahu 'alaihi wasallam dan apa yang dipegangi oleh para shahabat radliallahu anhum dalam perkara ushul (pokok) secara keseluruhannya, pokok-pokok tauhid , masalah kerasulan (kenabian), takdir, masalah-masalah iman dan selainnya.
Sementara yang selain mereka dari kelompok sempalan (yang menyempal/keluar dari jalan yang benar) seperti Khawarij, Mu`tazilah, Jahmiyah, Qadariyah, Rafidhah, Murji`ah dan pecahan dari kelompok-kelompok ini , semuanya merupakan ahlul bid`ah dalam perkara i`tiqad. Dan hukum yang dijatuhkan kepada mereka berbeda-beda, sesuai dengan jauh dekatnya mereka dari pokok-pokok agama, sesuai dengan keyakinan atau penafsiran mereka, dan sesuai dengan selamat tidaknya ahlus sunnah dari kejelekan pendapat dan perbuatan mereka. Dan perincian dalam permasalahan ini sangatlah panjang untuk dibawakan di sini.
Kedua : Bid`ah Amaliyah (bid`ah yang bersangkutan dengan amalan ibadah)
Bid`ah amaliyah adalah penetapan satu ibadah dalam agama ini padahal ibadah tersebut tidak disyariatkan oleh Allah dan Rasul-Nya. Dan perlu diketahui bahwasanya setiap ibadah yang tidak diperintahkan oleh Penetap syariat (yakni Allah ta`ala) baik perintah itu wajib ataupun mustahab (sunnah) maka itu adalah bid`ah amaliyah dan masuk dalam sabda nabi shallallahu alaihi wasallam :
"Siapa yang mengamalkan suatu amalan yang tidak di atas perintah kami maka amalannya itu tertolak".
Karena itulah termasuk kaidah yang dipegangi oleh para imam termasuk Imam Ahmad rahimahullah dan selain beliau menyatakan :
"Ibadah itu pada asalnya terlarang (tidak boleh dikerjakan)"
Yakni tidak boleh menetapkan/mensyariatkan satu ibadah kecuali apa yang disyariatkan oleh Allah dan Rasul-Nya.
Dan mereka menyatakan pula :
"Muamalah dan adat (kebiasaan) itu pada asalnya dibolehkan (tidak dilarang)"
Oleh karena itu tidak boleh mengharamkan sesuatu dari muamalah dan adat tersebut kecuali apa yang Allah ta`ala dan rasul-Nya haramkan. Sehingga termasuk dari kebodohan bila mengklaim sebagian adat yang bukan ibadah sebagai bid`ah yang tidak boleh dikerjakan, padahal perkaranya sebaliknya (yakni adat bisa dilakukan) maka yang menghukumi adat itu dengan larangan dan pengharaman dia adalah ahlu bid`ah (mubtadi). Dengan demikian, tidak boleh mengharamkan satu adat kecuali apa yang diharamkan oleh Allah dan Rasul-Nya.
Dan adat itu sendiri terbagi tiga :
Pertama : yang membantu mewujudkan perkara kebaikan dan ketaatan maka adat seperti ini termasuk amalan qurbah (yang mendekatkan diri kepada Allah).
Kedua : yang membantu/mengantarkan kepada perbuatan dosa dan permusuhan maka adat seperti ini termasuk perkara yang diharamkan.
Ketiga : adat yang tidak masuk dalam bagian pertama dan kedua (yakni tidak masuk dalam amalan qurbah dan tidak pula masuk dalam perkara yang diharamkan) maka adat seperti ini mubah (boleh dikerjakan). Wallahu a`lam.
Sabtu, 19 Juni 2010
HEPATITIS B
• The virus is transmitted through contact with the blood or other body fluids of an infected person - not through casual contact.
• About 2 billion people worldwide have been infected with the virus and about 350 million live with chronic infection. An estimated 600 000 persons die each year due to the acute or chronic consequences of hepatitis B.
• About 25% of adults who become chronically infected during childhood later die from liver cancer or cirrhosis (scarring of the liver) caused by the chronic infection.
• The hepatitis B virus is 50 to 100 times more infectious than HIV.
• Hepatitis B virus is an important occupational hazard for health workers.
• Hepatitis B is preventable with a safe and effective vaccine.
Hepatitis B is a potentially life-threatening liver infection caused by the hepatitis B virus. It is a major global health problem and the most serious type of viral hepatitis. It can cause chronic liver disease and puts people at high risk of death from cirrhosis of the liver and liver cancer.
Worldwide, an estimated two billion people have been infected with the hepatitis B virus (HBV), and more than 350 million have chronic (long-term) liver infections.
A vaccine against hepatitis B has been available since 1982. Hepatitis B vaccine is 95% effective in preventing HBV infection and its chronic consequences, and is the first vaccine against a major human cancer.
Symptoms
Hepatitis B virus can cause an acute illness with symptoms that last several weeks, including yellowing of the skin and eyes (jaundice), dark urine, extreme fatigue, nausea, vomiting and abdominal pain. People can take several months to a year to recover from the symptoms. HBV can also cause a chronic liver infection that can later develop into cirrhosis of the liver or liver cancer.
Who is most at risk for chronic disease?
The likelihood that an HBV infection will become chronic depends upon the age at which a person becomes infected, with young children who become infected with HBV being the most likely to develop chronic infections. About 90% of infants infected during the first year of life develop chronic infections; 30% to 50% of children infected between one to four years of age develop chronic infections. About 25% of adults who become chronically infected during childhood die from HBV-related liver cancer or cirrhosis.
About 90% of healthy adults who are infected with HBV will recover and be completely rid of the virus within six months.
Where is hepatitis B most common?
Hepatitis B is endemic in China and other parts of Asia. Most people in the region become infected with HBV during childhood. In these regions, 8% to 10% of the adult population are chronically infected. Liver cancer caused by HBV is among the first three causes of death from cancer in men, and a major cause of cancer in women. High rates of chronic infections are also found in the Amazon and the southern parts of eastern and central Europe. In the Middle East and Indian sub-continent, an estimated 2% to 5% of the general population is chronically infected. Less than 1% of the population in western Europe and North American is chronically infected.
Transmission
Hepatitis B virus is transmitted between people by contact with the blood or other body fluids (i.e. semen and vaginal fluid) of an infected person. Modes of transmission are the same for the human immunodeficiency virus (HIV), but HBV is 50 to 100 times more infectious Unlike HIV, HBV can survive outside the body for at least 7 days. During that time, the virus can still cause infection if it enters the body of a person who is not infected.
Common modes of transmission in developing countries are:
• perinatal (from mother to baby at birth)
• early childhood infections (inapparent infection through close interpersonal contact with infected household contacts)
• unsafe injections practices
• blood transfusions
• sexual contact
In many developed countries (e.g. those in western Europe and North America), patterns of transmission are different than those mentioned above. Today, the majority of infections in these countries are transmitted during young adulthood by sexual activity and injecting drug use. HBV is a major infectious occupational hazard of health workers.
HBV is not spread by contaminated food or water, and cannot be spread casually in the workplace.
The virus incubation period is 90 days on average, but can vary from about 30 to 180 days. HBV may be detected 30 to 60 days after infection and persist for widely variable periods of time.
Treatment
There is no specific treatment for acute hepatitis B. Care is aimed at maintaining comfort and adequate nutritional balance, including replacement of fluids that are lost from vomiting and diarrhoea.
Chronic hepatitis B can be treated with drugs, including interferon and anti-viral agents, which can help some patients. Treatment can cost thousands of dollars per year and is not available to most patients in developing countries.
Liver cancer is almost always fatal, and often develops in people at an age when they are most productive and have family responsibilities. In developing countries, most people with liver cancer die within months of diagnosis. In higher income countries, surgery and chemotherapy can prolong life for up to a few years in some patients.
Patients with cirrhosis are sometimes given liver transplants, with varying success.
Prevention
All infants should receive the hepatitis B vaccine: this is the mainstay of hepatitis B prevention.
The vaccine can be given as either three or four separate doses, as part of existing routine immunization schedules. In areas where mother-to-infant spread of HBV is common, the first dose of vaccine should be given as soon as possible after birth (i.e. within 24 hours).
The complete vaccine series induces protective antibody levels in more than 95% of infants, children and young adults. After age 40, protection following the primary vaccination series drops below 90%. At 60 years old, protective antibody levels are achieved in only 65 to 75% of those vaccinated. Protection lasts at least 20 years and should be lifelong.
All children and adolescents younger than 18 years old and not previously vaccinated should receive the vaccine. People in high risk groups should also be vaccinated, including:
• persons with high-risk sexual behaviour;
• partners and household contacts of HBV infected persons;
• injecting drug users;
• persons who frequently require blood or blood products;
• recipients of solid organ transplantation;
• those at occupational risk of HBV infection, including health care workers; and
• international travellers to countries with high rates of HBV.
The vaccine has an outstanding record of safety and effectiveness. Since 1982, over one billion doses of hepatitis B vaccine have been used worldwide. In many countries where 8% to 15% of children used to become chronically infected with HBV, vaccination has reduced the rate of chronic infection to less than 1% among immunized children.
As of December 2006, 164 countries vaccinate infants against hepatitis B during national immunization programmes - a major increase compared with 31 countries in 1992, the year that the World Health Assembly passed a resolution to recommend global vaccination against hepatitis B.
http://translate.google.co.id/translate?hl=id&sl=en&u=http://www.who.int/mediacentre/factsheets/fs204/en/&ei=ZXscTMDwBJGyrAfJyMimCw&sa=X&oi=translate&ct=result&resnum=4&ved=0CDEQ7gEwAw&prev=/search%3Fq%3DHBV%26hl%3Did%26sa%3DN

Jumat, 11 Juni 2010
SYSTEMIC LUPUS ERITEMATOSUS
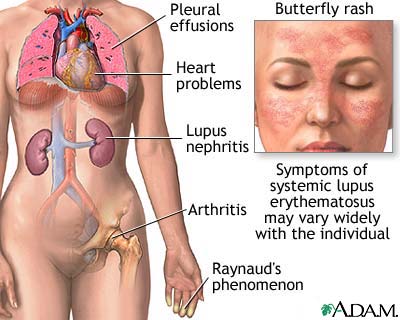
| DEFINISI Lupus Eritematosus Sistemik (Lupus Eritematosus Disseminata, Lupus) adalah suatu penyakit autoimun menahun yang menimbulkan peradangan dan bisa menyerang berbagai organ tubuh, termasuk kulit, persendian dan organ dalam. Pada setiap penderita, peradangan akan mengenai jaringan dan organ yang berbeda. Beratnya penyakit bervariasi mulai dari penyakit yang ringan sampai penyakit yang menimbulkan kecacatan, tergantung dari jumlah dan jenis antibodi yang muncul dan organ yang terkena. |
| PENYEBAB Dalam keadaan normal, sistem kekebalan berfungsi mengendalikan pertahanan tubuh dalam melawan infeksi. Pada lupus dan penyakit autoimun lainnya, sistem pertahanan tubuh ini berbalik melawan tubuh, dimana antibodi yang dihasilkan menyerang sel tubuhnya sendiri. Antibodi ini menyerang sel darah, organ dan jaringan tubuh, sehingga terjadi penyakit menahun. Mekanisme maupun penyebab dari penyakit autoimun ini belum sepenuhnya dimengerti. Penyebab dari lupus tidak diketahui, tetapi diduga melibatkan faktor lingkungan dan keturunan. Beberapa faktor lingkungan yang dapat memicu timbulnya lupus: Meskipun lupus diketahui merupakan penyakit keturunan, tetapi gen penyebabnya tidak diketahui. Penemuan terakhir menyebutkan tentang gen dari kromosom 1. Hanya 10% dari penderita yang memiliki kerabat (orang tua maupun saudara kandung) yang telah maupun akan menderita lupus. Statistik menunjukkan bahwa hanya sekitar 5% anak dari penderita lupus yang akan menderita penyakit ini. Lupus seringkali disebut sebagai penyakit wanita walaupun juga bisa diderita oleh pria. Lupus bisa menyerang usia berapapun, baik pada pria maupun wanita, meskipun 10-15 kali lebih sering ditemukan pada wanita. Faktor hormonal mungkin bisa menjelaskan mengapa lupus lebih sering menyerang wanita. Meningkatnya gejala penyakit ini pada masa sebelum menstruasi dan/atau selama kehamilan mendukung keyakinan bahwa hormon (terutama estrogen) mungkin berperan dalam timbulnya penyakit ini. Meskipun demikian, penyebab yang pasti dari lebih tingginya angka kejadian pada wanita dan pada masa pra-menstruasi, masih belum diketahui. Kadang-kadang obat jantung tertentu (hidralazin, prokainamid dan beta-bloker) dapat menyebabkan sindroma mirip lupus, yang akan menghilang bila pemakaian obat dihentikan. |
| GEJALA Jumlah dan jenis antibodi pada lupus, lebih besar dibandingkan dengan pada penyakit lain, dan antibodi ini (bersama dengan faktor lainnya yang tidak diketahui) menentukan gejala mana yang akan berkembang. Karena itu, gejala dan beratnya penyakit, bervariasi pada setiap penderita. Perjalanan penyakit ini bervariasi, mulai dari penyakit yang ringan sampai penyakit yang berat. Gejala pada setiap penderita berlainan, serta ditandai oleh masa bebas gejala (remisi) dan masa kekambuhan (eksaserbasi). Pada awal penyakit, lupus hanya menyerang satu organ, tetapi di kemudian hari akan melibatkan organ lainnya. Hampir semua penderita lupus mengalami nyeri persendian dan kebanyakan menderita artritis. Persendian yang sering terkena adalah persendian pada jari tangan, tangan, pergelangan tangan dan lutut. Kematian jaringan pada tulang panggul dan bahu sering merupakan penyebab dari nyeri di daerah tersebut. Pada 50% penderita ditemukan ruam kupu-kupu pada tulang pipi dan pangkal hidung. Ruam ini biasanya akan semakin memburuk jika terkena sinar matahari. Ruam yang lebih tersebar bisa timbul di bagian tubuh lain yang terpapar oleh sinar matahari. Sebagian besar penderita menunjukkan adanya penimbunan protein di dalam sel-sel ginjal, tetapi hanya 50% yang menderita nefritis lupus (peradangan ginjal yang menetap). Pada akhirnya bisa terjadi gagal ginjal sehingga penderita perlu menjalani dialisa atau pencangkokkan ginjal. Kelainan saraf ditemukan pada 25% penderita lupus. Yang paling sering ditemukan adalah disfungsi mental yang sifatnya ringan, tetapi kelainan bisa terjadi pada bagian manapun dari otak, korda spinalis maupun sistem saraf. Kejang, psikosa, sindroma otak organik dan sakit kepala merupakan beberapa kelainan sistem saraf yang bisa terjadi. Kelainan darah bisa ditemukan pada 85% penderita lupus. Bisa terbentuk bekuan darah di dalam vena maupun arteri, yang bisa menyebabkan stroke dan emboli paru. Jumlah trombosit berkurang dan tubuh membentuk antibodi yang melawan faktor pembekuan darah, yang bisa menyebabkan perdarahan yang berarti. Seringkali terjadi anemia akibat penyakit menahun. Peradangan berbagai bagian jantung bisa terjadi, seperti perikarditis, endokarditis maupun miokarditis. Nyeri dada dan aritmia bisa terjadi sebagai akibat dari keadaan tersebut. Pada lupus bisa terjadi pleuritis (peradangan selaput paru) dan efusi pleura (penimbunan cairan antara paru dan pembungkusnya). Akibat dari keadaan tersebut sering timbul nyeri dada dan sesak nafas.   Gejala dari penyakit lupus: - demam - lelah - merasa tidak enak badan - penurunan berat badan - ruam kulit - ruam kupu-kupu - ruam kulit yang diperburuk oleh sinar matahari - sensitif terhadap sinar matahari - pembengkakan dan nyeri persendian - pembengkakan kelenjar - nyeri otot - mual dan muntah - nyeri dada pleuritik - kejang - psikosa. Gejala lainnya yang mungkin ditemukan: - hematuria (air kemih mengandung darah) - batuk darah - mimisan - gangguan menelan - bercak kulit - bintik merah di kulit - perubahan warna jari tangan bila ditekan - mati rasa dan kesemutan - luka di mulut - kerontokan rambut - nyeri perut - gangguan penglihatan. |
| DIAGNOSA Diagnosis lupus ditegakkan berdasarkan ditemukannya 4 dari 11 gejala lupus yang khas, yaitu:
|
| PENGOBATAN Jika gejala lupus disebabkan karena obat, maka menghentikan penggunaan obat bisa menyembuhkannya, walaupun diperlukan waktu berbulan-bulan. Penyakit yang ringan (ruam, sakit kepala, demam, artritis, pleuritis, perikarditis) hanya memerlukan sedikit pengobatan. Untuk mengatasi artritis dan pleurisi diberikan obat anti peradangan non-steroid. Untuk mengatasi ruam kulit digunakan krim kortikosteroid. Untuk gejala kulit dan artritis kadang digunakan obat anti malaria (hydroxycloroquine). Jika penderita sangat sensitif terhadap sinar matahari, sebaiknya pada saat bepergian menggunakan tabir surya, pakaian panjang ataupun kacamata. Penyakit yang berat atau membahayakan jiwa penderitanya (anemia hemolitik, penyakit jantung atau paru yang meluas, penyakit ginjal, penyakit sistem saraf pusat) seringkali perlu ditangani oleh ahlinya. Untuk mengendalikan berbagai manifestasi dari penyakit yang berat mungkin bisa diberikan kortikosteroid atau obat penekan sistem kekebalan. Beberapa ahli memberikan obat sitotoksik (obat yang menghambat pertumbuhan sel) pada penderita yang tidak memberikan respon yang baik terhadap kortikosteroid atau yang tergantung kepada kortikosteroid dosis tinggi. PROGNOSIS Beberapa tahun terakhir ini prognosis penderita lupus semakin membaik, banyak penderita yang menunjukkan penyakit yang ringan. Wanita penderita lupus yang hamil dapat bertahan dengan aman sampai melahirkan bayi yang normal, tidak ditemukan penyakit ginjal ataupun jantung yang berat dan penyakitnya dapat dikendalikan. Angka harapan hidup 10 tahun meningkat sampai 85%. Prognosis yang paling buruk ditemukan pada penderita yang mengalami kelainan otak, paru-paru, jantung dan ginjal yang berat. |
Senin, 07 Juni 2010
Stevens-Johnson sindrom

Stevens–Johnson syndrome (SJS) is a form of erythema multiforme which is a life-threatening condition affecting the skin in which cell death causes the epidermis to separate from the dermis. The syndrome is thought to be a hypersensitivity complex affecting the skin and the mucous membranes. Although the majority of cases are idiopathic, the main class of known causes is medications, followed by infections and (rarely) cancers
Classification
There is agreement in the medical literature that Stevens–Johnson syndrome (SJS) can be considered a milder form of toxic epidermal necrolysis (TEN). These conditions were first recognised in 1922. Both diseases can be mistaken for erythema multiforme. Erythema multiforme is sometimes caused by a reaction to a medication but is more often a type IV hypersensitivity reaction to an infection (caused most often by Herpes simplex) and is relatively benign. Although both SJS and TEN can also be caused by infections, they are most often adverse effects of medications. Their consequences are potentially more dangerous than those of erythema multiforme.Signs and symptoms
SJS usually begins with fever, sore throat, and fatigue, which is misdiagnosed and usually treated with antibiotics. Ulcers and other lesions begin to appear in the mucous membranes, almost always in the mouth and lips but also in the genital and anal regions. Those in the mouth are usually extremely painful and reduce the patient's ability to eat or drink. Conjunctivitis of the eyes occurs in about 30% of children who develop SJS. A rash of round lesions about an inch across arises on the face, trunk, arms and legs, and soles of the feet, but usually not the scalp.Causes
SJS is thought to arise due to a disorder of the immune system.Infectious
It can be caused by infections (usually following infections such as herpes simplex virus, influenza, mumps, cat-scratch fever, histoplasmosis, Epstein-Barr virus, mycoplasma pneumoniae or similar).Medication/drugs
It can be due to adverse effects of drugs (allopurinol, diclofenac, etravirine, Isotretinoin, aka Accutane, fluconazole, valdecoxib, sitagliptin, oseltamivir, penicillins, barbiturates, sulfonamides, phenytoin, azithromycin, modafinil, lamotrigine, nevirapine, pyrimethamine, ibuprofen, ethosuximide, carbamazepine and gout medications)
Although Stevens–Johnson Syndrome can be caused by viral infections, malignancies or severe allergic reactions to medication, the leading cause appears to be the use of antibiotics and sulfa drugs.
Medications that have traditionally been known to lead to SJS, erythema multiforme and toxic epidermal necrolysis include sulfonamides (antibiotics), penicillins (antibiotics), barbiturates (sedatives), lamotrigine and phenytoin (e.g. Dilantin) (anticonvulsants). Combining lamotrigine with sodium valproate increases the risk of SJS.
Non-steroidal anti-inflammatory drugs are a rare cause of SJS in adults; the risk is higher for older patients, women and those initiating treatment. Typically, the symptoms of drug-induced SJS arise within a week of starting the medication. People with systemic lupus erythematosus or HIV infections are more susceptible to drug-induced SJS.
SJS has also been consistently reported as an uncommon side effect of herbal supplements containing ginseng. SJS may also be caused by cocaine usage.
Genetics
In some East Asian populations studied (Han Chinese and Thai), carbamazepine- and phenytoin-induced SJS is strongly associated with HLA-B*1502 (HLA-B75), an HLA-B serotype of the broader serotype HLA-B15.[10][11][12] A study in Europe suggested that the gene marker is only relevant for East Asians.[13][14] Based on the Asian findings, similar studies were performed in Europe which showed 61% of allopurinol-induced SJS/TEN patients carried the HLA-B58 (B*5801 allele - phenotype frequency in Europeans is typically 3%). One study concluded "even when HLA-B alleles behave as strong risk factors, as for allopurinol, they are neither sufficient nor necessary to explain the disease."
Treatment
SJS constitutes a dermatological emergency. All medications should be discontinued, particularly those known to cause SJS reactions. Patients with documented mycoplasma infections can be treated with oral macrolide or oral doxycycline.
Initially, treatment is similar to that for patients with thermal burns, and continued care can only be supportive (e.g. intravenous fluids and nasogastric or parenteral feeding) and symptomatic (e.g. analgesic mouth rinse for mouth ulcer). Dermatologists and surgeons tend to disagree about whether the skin should be debrided.
Beyond this kind of supportive care, there is no accepted treatment for SJS. Treatment with corticosteroids is controversial. Early retrospective studies suggested that corticosteroids increased hospital stays and complication rates. There are no randomized trials of corticosteroids for SJS, and it can be managed successfully without them.
Other agents have been used, including cyclophosphamide and cyclosporine, but none have exhibited much therapeutic success. Intravenous immunoglobulin (IVIG) treatment has shown some promise in reducing the length of the reaction and improving symptoms. Other common supportive measures include the use of topical pain anesthetics and antiseptics, maintaining a warm environment, and intravenous analgesics. An ophthalmologist should be consulted immediately, as SJS frequently causes the formation of scar tissue inside the eyelids, leading to corneal vascularization, impaired vision and a host of other ocular problems. Also, an extensive physical therapy program ensues after the patient is discharged from the hospital.
Prognosis
SJS proper (with less than 10% of body surface area involved) has a mortality rate of around 5%. The risk for death can be estimated using the SCORTEN scale, which takes a number of prognostic indicators into account. Other outcomes include organ damage/failure, cornea scratching and blindness.
Epidemiology
Stevens-Johnson syndrome is a rare condition, with a reported incidence of around 2.6 to 6.1 cases per million people per year. In the United States, there are about 300 new diagnoses per year. The condition is more common in adults than in children. Women are affected more often than men, with cases occurring at a three to two sex ratio.
- Typically, the disease process begins with a nonspecific upper respiratory tract infection.
- This usually is part of a 1- to 14-day prodrome during which fever, sore throat, chills, headache, and malaise may be present.
- Vomiting and diarrhea are occasionally noted as part of the prodrome.
- Mucocutaneous lesions develop abruptly. Clusters of outbreaks last from 2-4 weeks. The lesions are typically nonpruritic.
- A history of fever or localized worsening should suggest a superimposed infection; however, fever has been reported to occur in up to 85% of cases.
- Involvement of oral and/or mucous membranes may be severe enough that patients may not be able to eat or drink.
- Patients with genitourinary involvement may complain of dysuria or an inability to void.
- A history of a previous outbreak of Stevens-Johnson syndrome (SJS) or of erythema multiforme may be elicited. Recurrences may occur if the responsible agent is not eliminated or if the patient is reexposed.
- Typical symptoms are as follows:
- Cough productive of a thick purulent sputum
- Headache
- Malaise
- Arthralgia
- Physical
- The center of these lesions may be vesicular, purpuric, or necrotic.
- The typical lesion has the appearance of a target. The target is considered pathognomonic. However, in contrast to the typical erythema multiforme lesions, these lesions have only two zones of color. The core may be vesicular, purpuric, or necrotic; that zone is surrounded by macular erythema. Some have called these targetoid lesions.
- Lesions may become bullous and later rupture, leaving denuded skin. The skin becomes susceptible to secondary infection. Extensive sloughing is shown in the image below.
- Urticarial lesions typically are not pruritic.
- Infection may be responsible for the scarring associated with morbidity.
- Although lesions may occur anywhere, the palms, soles, dorsum of the hands, and extensor surfaces are most commonly affected. Desquamation on the foot is shown in the image below.
- The rash may be confined to any one area of the body, most often the trunk.
- Mucosal involvement may include erythema, edema, sloughing, blistering, ulceration, and necrosis. An example of this type of involvement is shown in the image below.
- Although some have suggested the possibility of Stevens-Johnson syndrome (SJS) without skin lesions, most believe that mucosal lesions alone are not enough to establish the diagnosis. Some are now calling cases without skin lesions "atypical" or "incomplete." This group of authors suggested that the combination of urethritis, conjunctivitis, and stomatitis made the diagnosis of SJS in a patient with Mycoplasma pneumoniae -induced signs and symptoms.
- The following signs may be noted on examination:
- Fever
- Orthostasis
- Tachycardia
- Hypotension
- Altered level of consciousness
- Epistaxis
- Conjunctivitis
- Corneal ulcerations
- Erosive vulvovaginitis or balanitis
- Seizures, coma
- The rash can begin as macules that develop into papules, vesicles, bullae, urticarial plaques, or confluent erythema.
Causes
- Drugs and malignancies are most often implicated as the etiology in adults and elderly persons.
- Pediatric cases are related more often to infections than to malignancy or a reaction to a drug.
- Oxicam NSAIDs and sulfonamides are most often implicated in western nations. In Southeast Asia, allopurinol is most common.
- A medication such as sulfa, phenytoin, or penicillin had previously been prescribed to more than two thirds of all patients with Stevens-Johnson syndrome (SJS). The anticonvulsant oxcarbazepine (Trileptal) has also been implicated. Hallgren et al reported ciprofloxacin-induced Stevens-Johnson syndrome in young patients in Sweden and commented on several others. Metry et al reported Stevens-Johnson syndrome in 2 HIV patients treated with nevirapine and mentioned one other in the literature. The authors speculated that the problem may extend to other non-nucleoside reverse transcriptase inhibitors. Indinavir has been mentioned.
- More than half of the patients with Stevens-Johnson syndrome report a recent upper respiratory tract infection.
- The 4 etiologic categories are (1) infectious, (2) drug-induced, (3) malignancy-related, and (4) idiopathic.
- Viral diseases that have been reported include herpes simplex virus (HSV), AIDS, coxsackie viral infections, influenza, hepatitis, mumps, lymphogranuloma venereum (LGV), rickettsial infections, and variola.
- Bacterial etiologies include group A beta streptococci, diphtheria, Brucellosis, mycobacteria, Mycoplasma pneumoniae, tularemia, and typhoid. An "incomplete" case was recently reported after Mycoplasma pneumoniae infection.
- Coccidioidomycosis, dermatophytosis, and histoplasmosis are the fungal possibilities.
- Malaria and trichomoniasis have been reported as protozoal causes.
- In children, Epstein-Barr virus and enteroviruses have been identified.
- Antibiotic etiologies include penicillins and sulfa antibiotics. Anticonvulsants including phenytoin, carbamazepine, valproic acid, lamotrigine, and barbiturates have been implicated. Mockenhapupt et al stressed that most anticonvulsant-induced SJS occurs in the first 60 days of use. In late 2002, the US Food and Drug Administration (FDA) and the manufacturer Pharmacia noted that Stevens-Johnson syndrome (SJS) had been reported in patients taking the cyclooxygenase-2 (COX-2) inhibitor valdecoxib. In 2007, the US FDA reported SJS/TEN in patients taking modafinil (Provigil). Allopurinol has recently been implicated as the most common cause in Europe and Israel.
- The most recent additions to possible drug-induced cases include the antidepressant mirtazapine and the TNF-alpha antagonists infliximab, etanercept, and adalimumab.
- Various carcinomas and lymphomas have been associated.
- Stevens-Johnson syndrome (SJS) is idiopathic in 25-50% of cases.
Senin, 31 Mei 2010
4 Fakta dan Mitos Tentang Shisha
Hanya karena prosedur dan alatnya lebih rumit, merokok dengan shisha sering dianggap lebih aman. Padahal selama yang dihisap adalah asap tembakau, racun nikotin tetap mengancam kesehatan. Berikut 4 fakta dan mitos soal shisha.
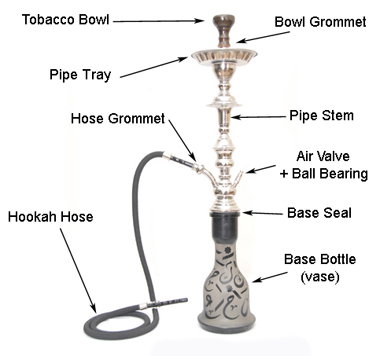
Shisha atau disebut juga hookah merupakan alat penghisap tembakau yang berasal dari India. Penggunaan alat ini populer di Timur Tengah, dan menyebar ke seluruh dunia.
Bentuk alat ini mirip lampu minyak, dengan tabung utama yang terhubung ke sejumlah pipa penghisap. Papan pemanas berisi bara api terdapat di bagian paling atas, berfungsi untuk membakar tembakau.
Tabung utama biasanya terbuat dari kaca, dan berisi air sebagai filter. Karena filternya berupa air, maka muncullah anggapan bahwa shihsa lebih aman dibandingkan rokok filter.
Dikutip dari Live Science, Senin (31/5/2010), sebuah penelitian di Inggris berhasil mementahkan anggapan tersebut. Penelitian yang dilakukan tahun 2009 itu dimuat dalam American Journal of Preventive Medicine.
Menurut penelitian tersebut, shisha justru menghasilkan asap lebih banyak dibandingkan rokok. Akibatnya, karbon monoksida (CO) yang terhirup lebih banyak dan bisa menyebabkan sesak napas.
Kadar nikotin pada shisha juga tidak lebih sedikit meski difilter dengan air. Secara umum risiko kesehatan yang dihadapi saat menghisap shisha sama besarnya dengan rokok biasa, termasuk kanker paru-paru serta gangguan kehamilan.
Oleh karena itu, pikirkan sekali lagi jika masih menganggap shisha lebih aman dibandingkan rokok. Berikut ini adalah 4 mitos paling populer di kalangan pengguna shisha, dikutip dari Live Science, Senin (31/5/2010).
Mitos: Shisha menghasilkan nikotin lebih sedikit dibandingkan rokok biasa.
Fakta: Penelitian di atas membuktikan, shisha maupun rokok biasa menghasilkan nikotin dalam kadar yang kurang lebih sama. Kalaupun ada perbedaan, itu tergantung pada tembakaunya dan biasanya shisha justru menggunakan tembakau terbaik dengan kadar nikotin lebih tinggi.
Mitos: Asap yang lebih tipis menunjukkan kadar racun pada shisha lebih kecil.
Fakta: Asap yang tipis pada shisha disebabkan oleh kelembaban yang tinggi, karena adanya air. Kadar racun tidak terpengaruh oleh ketebalan asap.
Mitos: Air di dasar shisha berfungsi sebagai filter racun.
Fakta: Dalam jumlah sangat kecil, memang ada racun yang terjebak dalam air. Tetapi jumlahnya tidak signifikan untuk menekan risiko kesehatan yang bisa muncul.
Mitos: Tembakau dengan rasa buah-buahan yang sering digunakan dengan shisha memberi manfaat bagi kesehatan.
Fakta: Fungsi bahan perasa yang digunakan hanya untuk aroma, sedikitpun tidak memberi manfaat bagi kesehatan.
Rabu, 26 Mei 2010
Mucus / Lendir
In vertebrates, mucus (adjectival form: "mucous") is a slippery secretion produced by, and covering, mucous membranes. It is a viscous colloid containing antiseptic enzymes (such as lysozyme), proteins such as lactoferrin, glycoproteins known as mucins that are produced by goblet cells in the mucous membranes and submucosal glands, immunoglobulins, and inorganic salts. This mucus serves to protect epithelial cells in the respiratory, gastrointestinal, urogenital, visual, and auditory systems in mammals; the epidermis in amphibians; and the gills in fish. A major function of this mucus is to protect against infectious agents such as fungi, bacteria and viruses. The average human body produces about a litre of mucus per day.
Snails, slugs, bony fish, hagfish and some other invertebrates also produce external mucus. In addition to serving a protective function against infectious agents, such mucus provides protection against toxins produced by predators, can facilitate movement and may play a role in communication.
Respiratory system
In the respiratory system mucus aids in the protection of the lungs by trapping foreign particles that enter it, particularly through the nose, during normal breathing. "Phlegm" is a specialized term for mucus that is restricted to the respiratory tract, while the term "mucus" more globally describes secretions of the nasal passages as well.
Nasal mucus is produced by the nasal mucosa, and mucal tissues lining the airways (trachea, bronchus, bronchioles) is produced by specialized airway epithelial cells (goblet cells) and submucosal glands. Small particles such as dust, particulate pollutants, and allergens as well as infectious agents such as bacteria are caught in the viscous nasal or airway mucus and prevented from entering the system. This event along with the continual movement of the respiratory mucus layer toward the oropharynx, helps prevent foreign objects from entering the lungs during breathing. Additionally, mucus aids in moisturizing the inhaled air and prevents tissues such as the nasal and airway epithelia from drying out. Nasal and airway mucus is produced constitutively, with most of it swallowed unconsciously, even when it is dried.
Increased mucus production in the respiratory tract is a symptom of many common illnesses, such as the common cold and influenza. Similarly, hypersecretion of mucus can occur in inflammatory respiratory diseases such as respiratory allergies, asthma, and chronic bronchitis. The presence of mucus in the nose and throat is normal, but increased quantities can impede comfortable breathing and must be cleared by blowing the nose or expectorating phlegm from the throat. Tears are also a component of nasal mucus.
Diseases involving mucus
Generally nasal mucus is clear and thin, serving to filter air during inhalation. During times of infection, mucus can change colour to yellow or green either as a result of trapped bacteria, or due to the body's reaction to viral infection.
In the case of bacterial infection, the bacterium becomes trapped in already clogged sinuses, breeding in the moist, nutrient-rich environment. Antibiotics may be used to treat the secondary infection in these cases, but will generally not help with the original cause.
In the case of a viral infection such as cold or flu, the first stage and also the last stage of the infection causes the production of a clear, thin mucus in the nose or back of the throat. As the body begins to react to the virus (generally one to three days), mucus thickens and may turn yellow or green. In viral infections, antibiotics will not be useful, and are a major avenue for misuse. Treatment is generally symptom-based; often it is sufficient to allow the immune system to fight off the virus over time.
Mucus as a medical symptom
Increased mucus production in the upper respiratory tract is a symptom of many common ailments, such as the common cold. Nasal mucus may be removed by blowing the nose, picking the nose, or by using traditional methods of nasal irrigation. Excess nasal mucus, as with a cold or allergies may be treated cautiously with decongestant medications. Excess mucus production in the bronchi and bronchioles, as may occur in asthma, bronchitis or influenza, may be treated with anti-inflammatory medications as a means of reducing the airway inflammation which triggers mucus over-production. Thickening of mucus as a "rebound" effect following overuse of decongestants may produce nasal or sinus drainage problems and circumstances that promote infection. Mucus with any color other than clear or white is generally an indicator of an infection of the nasal mucosa, the paranasal sinus or, if produced via a productive cough, of a lower respiratory tract infection.
Cold weather and mucus
During cold weather, the cilia which normally sweep mucus away from the nostrils and towards the back of the throat (see respiratory epithelium) become sluggish or completely cease functioning. This results in mucus running down the nose and dripping (a runny nose). Mucus also thickens in cold weather; when an individual comes in from the cold, the mucus thaws and begins to run before the cilia begin to work again.
Digestive system
In the digestive system, mucus is used as a lubricant for materials which must pass over membranes, e.g., food passing down the esophagus. A layer of mucus along the inner walls of the stomach is vital to protect the cell linings of that organ from the highly acidic environment within it. The same protective layer of mucus is what comes out when you sneeze. Mucus does not digest in the intestinal tract, so mucus commonly appears in fecal matter whether its origin is from the intestines, or swallowed.
Reproductive system
In the female reproductive system, cervical mucus prevents infection. The consistency of cervical mucus varies depending on the stage of a woman's menstrual cycle. At ovulation cervical mucus is clear, runny, and conducive to sperm; post-ovulation, mucus becomes thicker and is more likely to block sperm.
In the male reproductive system, the seminal vesicles contribute up to 60% of the total volume of the semen and contain mucus, amino acids, and fructose as the main energy source for the sperm.
BERSIN JUGA SEHAT

Sebagian orang mungkin menganggap bersin adalah hal sepele. Padahal, bersin merupakan suatu mekanisme pertahanan tubuh untuk mencegah masuknya zat asing ke dalam tubuh. Karena itu jangan ditahan jika anda terasa ingin bersin.
Selain menyebabkan kuman dan benda asing tertahan dalam tubuh, menahan bersin juga menyebabkan beberapa hal lainnya. Misalnya pecahnya gendang telinga, kehilangan pendengaran, Pembengkakan wajah sementara dan keretakan tulang rawan hidung. Sebab, saluran hidung dan mulut yang menjadi sarana keluaran bersin berhubungan juga dengan telinga.
Untuk diketahui, bersin adalah respon tubuh yang dilakukan oleh membran hidung ketika mendeteksi adanya bakteri dan kelebihan cairan yang masuk ke dalam hidung, sehingga secara otomatis tubuh akan menolak bakteri tersebut. Bersin juga dapat timbul akibat adanya peradangan (rhinosinusitis), benda asing, infeksi virus, atau reaksi alergi. Reaksi alergi tersebut muncul karena paparan terhadap bahan alergen.
Selain karena alergi, gejala pada hidung tersebut disebabkan bahan-bahan nonalergi yang ditimbulkan faktor lingkungan. Di antaranya, perubahan udara, temperatur, suhu, kelembapan, tekanan udara, atau bahan-bahan kimia dari obat-obat atau kosmetik tertentu. Mungkin juga akibat polusi udara karena asap kendaraan dan lingkungan industri. Kepantasan udara yang dilepaskan ketika bersin bisa mencapai 160 km/jam.
Kamis, 20 Mei 2010
Pasteurization / Pasteurisasi
Pasteurization is not intended to destroy all pathogenic micro-organisms in the food or liquid. Instead, pasteurization aims to reduce the number of viable pathogens so they are unlikely to cause disease (assuming pasteurization product is stored as indicated and consumed before its expiration date). Commercial-scale sterilisation of food is not common because it adversely affects the taste and quality of the product. Certain food products are processed to achieve the state of commercial sterility.
Products that can be pasteurized
- Almonds
- Apple cider
- Beer
- Canned food
- Cheese
- Cornbread
- Crabs
- Cream
- Eggs
- Honey (not necessary unless it is diluted)
- Juice
- Maple Syrup
- Milk
- Palm wine
- Ready Meal
- Soy sauce
- Sports drinks
- Tobacco
- Vinegar
- Water
- Wine
Pasteurisasi adalah sebuah proses pemanasan makanan dengan tujuan membunuh organisme merugikan seperti bakteri, virus, protozoa, kapang, dan khamir. Proses ini diberi nama atas penemunya Louis Pasteur seorang ilmuwan Perancis. Tes pasteurisasi pertama diselesaikan oleh Pasteur dan Claude Bernard pada 20 April 1862.
Tidak seperti sterilisasi, pasteurisasi tidak dimaksudkan untuk membunuh seluruh mikroorganisme di makanan. Bandingkan dengan appertisasi yang diciptakan oleh Nicolas Appert. Pasteurisasi bertjujuan untuk mencapai "pengurangan log" dalam jumlah organisme, mengurangi jumlah mereka sehingga tidak lagi bisa menyebabkan penyakit (dengan syarat produk yang telah dipasteurisasi didinginkan dan digunakan sebelum tanggal kadaluwarsa). Sterilisasi skala komersial makanan masih belum umum, karena dia mempengaruhi rasa dan kualitas dari produk.
Produk yang bisa dipasteurisasi
- susu
- anggur
- bir
- jus buah
- cider (sari buah apel)
- madu
- telur
- minuman olah raga
- makanan kaleng
Rabu, 19 Mei 2010
Woolsorter’s disease or Anthrax
 Woolsorter’s disease was also once known as ragpicker’s disease; its most common form in humans is cutaneous infection via the injured skin or mucous membranes of agricultural or industrial workers associated with infected animals or animal products. In 1877, the bacillus was the first bacterium shown to be the cause of a disease—one of the origins of the famous (Robert) Koch’s postulates. Along with mad cow disease, toxoplasmosis and the black plague ,anthrax is one of many animal blights with a direct impact on human health. The disease is surprisingly common and is endemic in the United States, EROPA, ASIA, AFRIKA, KARIBIA
Woolsorter’s disease was also once known as ragpicker’s disease; its most common form in humans is cutaneous infection via the injured skin or mucous membranes of agricultural or industrial workers associated with infected animals or animal products. In 1877, the bacillus was the first bacterium shown to be the cause of a disease—one of the origins of the famous (Robert) Koch’s postulates. Along with mad cow disease, toxoplasmosis and the black plague ,anthrax is one of many animal blights with a direct impact on human health. The disease is surprisingly common and is endemic in the United States, EROPA, ASIA, AFRIKA, KARIBIA
Infection occurs through the skin or by inhalation or ingestion of bacterial spores. Intestinal and pulmonary anthrax are the most deadly. The latter usually results in death 1–2 days after the onset of acute symptoms. Treatment with antibiotics such as penicillin is generally effective after initial exposure and can protect against growing bacilli, but it will not destroy the spores themselves.
The bacteria can propagate wildly and stimulate effusions of blood and fluids in various organs and body cavities (>109 bacteria/mL of blood is commonplace). This is followed by prostration of the victim and organ failure. One of the reasons anthrax is such a deadly pathogen may be because its evolution has made it dependent on the death of the host for propagation. Once death ensues in nature, the animal’s carcass rots in the field, exposing the bacteria crowded in the bloodstream to the open air. This stimulates spore formation, which is the main transmissible source of the disease. Spores can survive for decades in contaminated soil from which they can ultimately be inhaled or ingested by herbivores, which starts the cycle over again. Because anthrax requires the death of its host to effect transmission, few evolutionary stops exist compared with disease organisms that depend on the host staying alive—at least long enough for transmission.
Vaccine controversy
Normally, anthrax vaccination is only recommended for workers in danger of exposure—especially farmworkers and veterinarians in rural practice. But anthrax has also been a staple of the biological warfare arsenal for nearly 60 years; thus, it is increasingly a military concern. Ever since the Gulf War and the decision by the U.S. military to conduct mandatory anthrax vaccinations of its personnel, there has been public controversy over the safety and efficacy of the vaccine. A recent U.S. Supreme Court decision upheld the right of the military to enforce its anthrax vaccination policy. Studies conducted by the Centers for Disease Control and Prevention (CDC) found no link between anthrax vaccination and adverse reactions, including the purported “Gulf War Syndrome”.As part of a congressionally mandated CDC Anthrax Vaccine Research Program, new studies on rhesus monkeys are planned to determine the vaccine’s effectiveness, especially against aerosol delivery, the most likely terrorist scenario.
The only approved anthrax vaccine in the United States is produced from a cell-free filtrate of bacterial cultures. Vaccination generally involves a 6-dose schedule at 0, 2, and 4 weeks with boosters at 6, 12, and 18 months. Problems with vaccine supply have also recently been an issue—BioPort Corp., the Lansing, MI, company that makes the vaccine, was unable to produce sufficient doses to meet demand in 2000.For the CDC’s view of the vaccine issue, visit the CDC Web site, especially >www.cdc.gov/mmwr/preview/mmwrhtml/rr4915a1.htm.
INHALATION ANTRHAX

CUTANEOUS ANTHRAX

Minggu, 16 Mei 2010
ANTIGENIC DRIFT AND ANTEGENIC SHIFT

Antigenic drift: A mechanism for variation by viruses that involves the accumulation of mutations within the antibody-binding sites so that the resulting viruses cannot be inhibited well by antibodies against previous strains making it easier for them to spread throughout a partially immune population.
Antigenic drift occurs in both influenza A and influenza B viruses.
Antigenic drift: Sebuah mekanisme untuk variasi oleh virus yang melibatkan akumulasi mutasi dalam situs mengikat antibodi sehingga virus yang dihasilkan tidak dapat dihambat dengan baik oleh antibodi terhadap strain sebelumnya sehingga lebih mudah bagi mereka untuk tersebar di seluruh kekebalan sebagian penduduk. Antigenic drift terjadi di kedua influenza A dan B virus influenza
Antigenic shift: A sudden shift in the antigenicity of a virus resulting from the recombination of the genomes of two viral strains. Antigenic shift is seen only with influenza A viruses. It results usually from the replacement of the hemagglutinin (the viral attachment protein that also mediates the entry of the virus into the cell) with a novel subtype that has not been present in human influenzaviruses for a long time. The source of these new genes is the large reservoir of influenzaviruses in waterfowl. The consequences of the introduction of a new hemagglutinin into human viruses is usually a pandemic, or a worldwide epidemic.
Antigenic shift: Perubahan mendadak dalam antigenicity dari virus yang dihasilkan dari rekombinasi genom dari dua galur virus. Pergeseran antigenik terlihat hanya dengan virus influenza A. Itu biasanya hasil dari penggantian hemaglutinin (lampiran protein virus yang juga menengahi masuknya virus ke dalam sel) dengan subtipe novel yang tidak pernah hadir di influenzaviruses manusia untuk waktu yang lama. Sumber gen ini baru merupakan reservoir yang besar influenzaviruses di unggas air. Konsekuensi dari penerapan suatu hemaglutinin baru ke dalam virus manusia biasanya merupakan pandemi, atau epidemi di seluruh dunia.
Kamis, 13 Mei 2010
ATHLETE'S FOOT / TINEA PEDIS

Athlete's foot ( of the foot and tinea pedis) is a fungal infection of the skin that causes scaling, flaking, and itch of affected areas. It is caused by fungi in the genus Trichophyton and is typically transmitted in moist areas where people walk barefoot, such as showers or bathhouses. Although the condition typically affects the feet, it can spread to other areas of the body, including the groin. Athlete's foot can be prevented by good hygiene, and is treated by a number of pharmaceutical and other treatments.
Symptoms
Athlete's foot causes scaling, flaking, and itching of the affected skin. Blisters and cracked skin may also occur, leading to exposed raw tissue, pain, swelling, and inflammation. Secondary bacterial infection can accompany the fungal infection, sometimes requiring a course of oral antibiotics.
The infection can be spread to other areas of the body, such as the groin, and usually is called by a different name once it spreads, such as tinea corporis on the body or limbs and tinea cruris (jock itch or dhobi itch) for an infection of the groin. Tinea pedis most often manifests between the toes, with the space between the fourth and fifth digits most commonly afflicted.
Some individuals may experience an allergic response to the fungus called an "id reaction" in which blisters or vesicles can appear in areas such as the hands, chest and arms. Treatment of the fungus usually results in resolution of the id reaction.
Diagnosis
Diagnosis & treatment can be performed by a general practitioner or pharmacist, and by specialists such as a dermatologist, podiatrist & to a lesser extent a foot health practitioner .
Athlete's foot can usually be diagnosed by visual inspection of the skin, but where the diagnosis is in doubt direct microscopy of a potassium hydroxide preparation (known as a KOH test) may help rule out other possible causes, such as eczema or psoriasis. A KOH preparation is performed on skin scrapings from the affected area. The KOH preparation has an excellent positive predictive value, but occasionally false negative results may be obtained, especially if treatment with an anti-fungal medication has already begun.
If the above diagnoses are inconclusive or if a treatment regimen has already been started, a biopsy of the affected skin (i.e. a sample of the living skin tissue) can be taken for histological examination.
A Wood's lamp, although useful in diagnosing fungal infections of the hair (Tinea capitis), is not usually helpful in diagnosing tinea pedis since the common dermatophytes that cause this disease do not fluoresce under ultraviolet light. However, it can be useful for determining if the disease is due to a non-fungal afflictor.
Transmission
From person to person
Athlete's foot is a communicable disease caused by a parasitic fungus in the genus Trichophyton, either Trichophyton rubrum or Trichophyton mentagrophytes.[8] It is typically transmitted in moist environments where people walk barefoot, such as showers, bath houses, and locker rooms. It can also be transmitted by sharing footwear with an infected person, or less commonly, by sharing towels with an infected person.
To other parts of the body
The various parasitic fungi that cause athlete's foot can also cause skin infections on other areas of the body, most often under toenails (onychomycosis) or on the groin (tinea cruris).
Prevention
The practices given in this section do not only help prevent spread of the fungus, they can also help greatly in managing and curing athlete's foot in an individual by reducing or eliminating re-exposure to the fungus in one's home environment.
The fungi that cause athlete's foot can live on shower floors, wet towels, and footwear. Athlete's foot is caused by a fungus and can spread from person to person from shared contact with showers, towels, etc. Hygiene therefore plays an important role in managing an athlete's foot infection. Since fungi thrive in moist environments, it is very important to keep feet and footwear as dry as possible.
Prevention measures in the home
The fungi that cause athlete's foot live on moist surfaces and can be transmitted from an infected person to members of the same household through secondary contact.[12] By controlling the fungus growth in the household, transmission of the infection can be prevented.
Bathroom hygiene
* Spray tub and bathroom floor with disinfectant after each use to help prevent reinfection and infection of other household members.
Frequent laundering
* Wash sheets, towels, socks, underwear, and bedclothes in hot water (at 60 °C / 140 °F) to kill the fungus.
* Change towels and bed sheets at least once per week.
Avoid sharing
* Avoid sharing of towels, shoes and socks between household members.
* Use a separate towel for drying infected skin areas.
Prevention measures in public places
* Wear shower shoes or sandals in locker rooms, public showers, and public baths.
* Wash feet, particularly between the toes, with soap and dry thoroughly after bathing or showering.
* If you have experienced an infection previously, you may want to treat your feet and shoes with over-the-counter drugs.
Personal prevention measures
* Dry feet well after showering, paying particular attention to the web space between the toes.
* Try to limit the amount that your feet sweat by wearing open-toed shoes or well-ventilated shoes, such as lightweight mesh running shoes. Some shoes (such as the Geox brand) are specifically marketed as breathable and may help keep feet dry.
* Wear lightweight cotton socks to help reduce sweat. These must be washed in hot water and/or bleached to avoid reinfection. New light weight, moisture wicking polyester socks, especially those with anti-microbial properties, may be a better choice. Bamboo socks are claimed to be much more absorbent than cotton and so may help keep feet dry.
* Use foot powder to help reduce moisture and friction. Some foot powders also include an anti-fungal ingredient.
* Keep feet dry using an antiperspirant (not just a deodorant). If hyperhydrosis (excess sweating) is an issue use an antiperspirant with a higher concentration of active ingredients (e.g. 20% aluminium chloride hexahydrate).
* Keep shoes dry by wearing a different pair each day.
* Sanitize the inside of your shoes with a germicidal shoe tree.
* Change socks and shoes after exercise.
* Replace sole inserts in shoes/sneakers on a frequent basis.
* Replace old sneakers and exercise shoes.
* After any physical activity shower with a soap that has both an antibacterial and anti-fungal agent in it.
Treatments
There are many conventional medications (over-the-counter and prescription) as well as alternative treatments for fungal skin infections, including athlete's foot. Important with any treatment plan is the practice of good hygiene. Several placebo controlled studies report that good foot hygiene alone can cure athlete's foot even without medication in 30-40% of the cases. However, placebo-controlled trials of allylamines and azoles for athlete’s foot consistently produce much higher percentages of cure than placebo.
Since athlete's foot thrives in moist environments it is important for individuals with hyperhidrosis to reduce excess sweating.
Conventional treatments
Conventional treatment typically involves daily or twice daily application of a topical medication in conjunction with hygiene measures outlined in the above section on prevention. Keeping feet dry and practicing good hygiene is crucial to preventing reinfection. Severe or prolonged fungal skin infections may require treatment with oral anti-fungal medication. Zinc oxide based diaper rash ointment may be used; talcum powder can be used to absorb moisture to kill off the infection.
Topical medications
The fungal infection is often treated with topical antifungal agents, which can take the form of a spray, powder, cream, or gel. The most common ingredients in over-the-counter products are miconazole nitrate (2% typical concentration in the United States) and tolnaftate (1% typ. in the U.S.). Terbinafine is another common over-the-counter drug. There exists a large number of prescription antifungal drugs, from several different drug families. These include ketaconazole, itraconazole, naftifine, nystatin,
Some topical applications such as carbol fuchsin (also known in the U.S. as Castellani's paint), often used for intertrigo, work well but in small selected areas. This red dye, used in this treatment like many other vital stains, is both Fungicide. But still the number one thing to curing athletes foot is to have good hygiene.
The time line for cure may be long, often 45 days or longer. The recommended course of treatment is to continue to use the topical treatment for four weeks after the symptoms have subsided to ensure that the fungus has been completely eliminated. However, because the itching associated with the infection subsides quickly, patients may not complete the courses of therapy prescribed.
Anti-itch creams are not recommended as they will alleviate the symptoms but will exacerbate the fungus; this is due to the fact that anti-itch creams typically enhance the moisture content of the skin and encourage fungal growth. For the same reason, some drug manufacturers are using a gel instead of a cream for application of topical drugs (for example, naftin and Lamisil). Novartis, maker of Lamisil, claims that a gel penetrates the skin more quickly than cream.
If the fungal invader is not a dermatophyte but a yeast, other medications such as fluconazole may be used. Typically fluconazole is used for candidal vaginal infections moniliasis but has been shown to be of benefit for those with cutaneous yeast infections as well. The most common of these infections occur in the web spaces (intertriginous) of the toes and at the base of the fingernail or toenail. The hall mark of these infections is a cherry red color surrounding the lesion and a yellow thick pus.
Oral medications
Oral treatment with griseofulvin was begun early in the 1950s. Because of the tendency to cause liver problems and to provoke aplastic anemia the drugs were used cautiously and sparingly. Over time it was found that those problems were due to the size of the crystal in the manufacturing process and microsize and now ultramicrosize crystals are available with few of the original side effects.[citation needed]
For severe cases, the current preferred oral agent in the UK is the more effective terbinafine. Other prescription oral antifungals include itraconazole and fluconazole.
Alternative treatments
Topical oils
Symptomatic relief from itching may be achieved after topical application of tea tree oil, probably due to its involvement in the histamine response; however, the efficacy of tea tree oil in the treatment of athlete's foot (achieving mycological cure) is varied.
Onion extract
A study of the effect of 3% (v/v) aqueous onion extract was shown to be very effective in laboratory conditions against Trichophyton mentagrophytes and T. rubrum.
Garlic extract
Ajoene, a compound found in garlic, is sometimes used to treat athlete's foot.
Boric acid
Boric acid application in the socks is used to prevent athlete's foot when recurrent infections occurs, but is not used to treat it.
Epsom salts
Some podiatrists recommend soaking the feet in a solution of Epsom salts in warm water.
Nah,,mumpung slama ini artikel saya pake bahasa Indonesia, kan yg mengunjungi blokg saya dan butuh pengetahuan bukan cuma oramg indonesia, jadi mulai sekarang artikel saya ada yg menggunakan bhasa inggris dan ada yg menggunakan bahasa Indonesia, klo artikelnya sedikit, saya pake dua2nya...sekalian melatih bahasa Para Pembaca dan saya trima kasih ^^, thanks you ^^, arigatou gozaimazu,, ^^


